Increasing Workforce Productivity in the Diagnostic Laboratory





NHS Tayside Workflow Optimization. Jeff Appleyard, Siemens Healthineers
FierceHealthcare. Hospital CFOs need more data on labor costs. (https://www.fiercehealthcare.com/finance/hospital-cfos-need-more-data-labor-costs)
The Lewin Group, Inc. The value of diagnostics innovation, adoption and diffusion into health care. 2005. (https://dx.advamed.org/sites/dx.advamed.org/files/resource/Lewin%20Value%20of%20Diagnostics%20Report.pdf)
CLMA. The laboratory personnel shortage. (http://www.ascls.org/images/Government_AffairsGAC/AHRA.pdf?_sm_au_=iVVN0T5trV0TssT0)
Health Services Research. Predicting Changes in Staff Morale and Burnout at Community Health Centers Participating in the Health Disparities Collaboratives.2008 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2517268/)
Asian Pacific Journal of Tropical Biomedicine. Challenges of a negative work load and implications on morale, productivity and quality of service delivered in NHS laboratories in England. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3994349/)
Reuters Health News. Reimbursement cuts on lab tests pressure U.S. lab firm shares. (https://www.reuters.com/article/us-usa-healthcare-medicare/reimbursement-cuts-on-lab-tests-pressure-u-s-lab-firm-shares-idUSKBN1DK25J)
Murphy Leadership Institute. Research brief: Eliminating wasteful work in hospitals improves margin, quality and culture (http://www.cs.odu.edu/~cpi/old/cpi-s2004/statag/murphy-wastefulwork.pdf?_sm_au_=iVVN0T5trV0TssT0)
Elsevier. Nurse staffing levels and the incidence of mortality and morbidity in the adult intensive care unit: a literature review. 2012. (https://www.sciencedirect.com/science/article/pii/S1036731412000471)
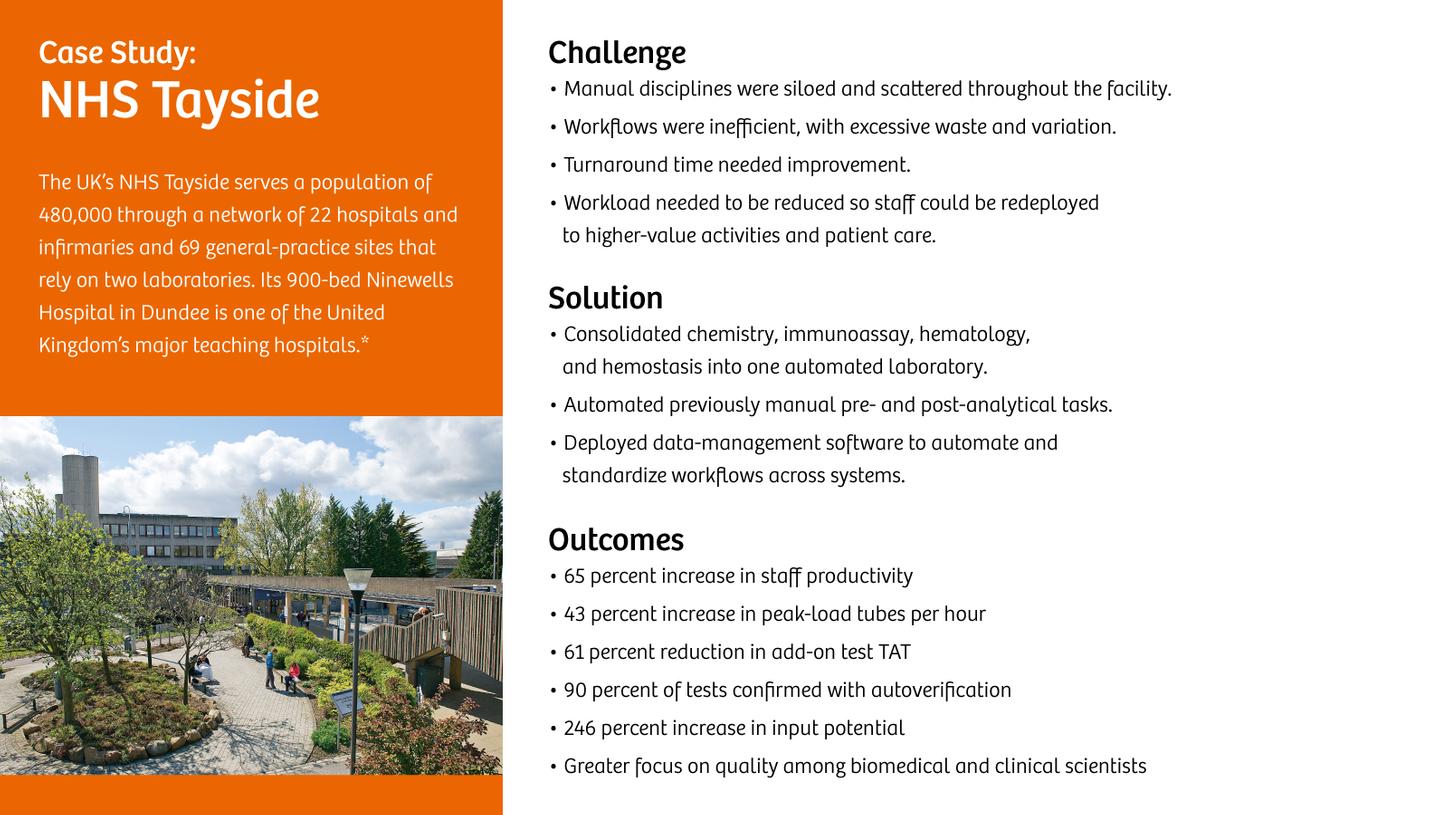
* The outcomes obtained by the Siemens Healthineers customer described here were realized in the customer’s unique setting.
Since there is no typical laboratory, and many variables exist, there can be no guarantee that others will achieve the same results.